Effective charting and documentation are critical components of patient care and legal protection for healthcare providers. Nurse practitioners must master these skills to ensure accurate patient records, continuity of care, and compliance with regulatory standards. While charting and documentation can sometimes feel overwhelming, employing the right strategies can make the process more efficient and effective.
Why Charting and Documentation Matter
Charting and documentation serve multiple purposes in the healthcare setting. They provide a comprehensive record of a patient’s history, treatments, and progress, ensuring seamless communication among healthcare providers. Additionally, they serve as a legal safeguard, demonstrating that appropriate care was provided. For a nurse practitioner, thorough and precise documentation can protect against malpractice claims and regulatory scrutiny.
Essential Charting and Documentation Tips
1. Follow the SOAP Format
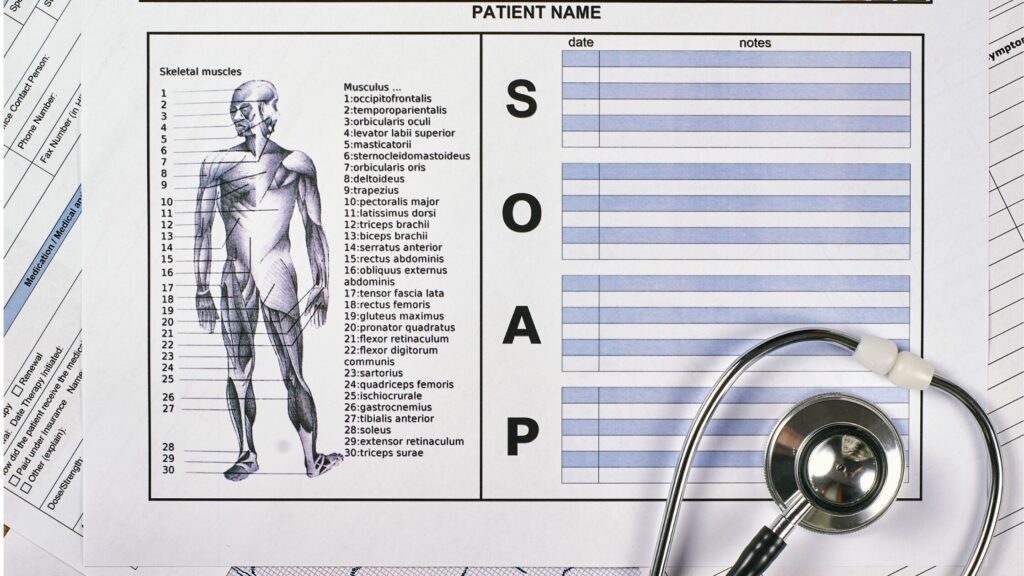
One of the most effective ways to structure patient notes is by using the SOAP format:
- Subjective: The patient’s description of symptoms and concerns.
- Objective: Measurable findings from physical exams, lab results, and imaging.
- Assessment: Diagnosis or clinical impressions based on subjective and objective data.
- Plan: Treatment plan, follow-up instructions, and next steps.
The SOAP format ensures that charting and documentation are organized, making it easier for other providers to understand and continue patient care seamlessly.
2. Be Clear, Concise, and Objective
Avoid ambiguous language or excessive detail. Instead, use precise terminology and factual statements. For example, rather than writing “Patient appears to be in pain,” document “Patient reports sharp pain in the right lower abdomen, rated 7/10.” This level of specificity improves communication and provides a clearer clinical picture.
3. Use Approved Abbreviations and Terminology
Healthcare organizations have approved abbreviations to maintain consistency and clarity. Nurse practitioners should be familiar with their institution’s list of accepted abbreviations and avoid using ambiguous shorthand that could lead to misinterpretation.
4. Document in Real-Time
Delayed documentation increases the risk of missing important details. Aim to complete charting and documentation as soon as possible after seeing a patient. If immediate charting isn’t feasible, jot down key points and complete the record as soon as time allows.
5. Maintain Accuracy and Integrity
Never alter or falsify documentation. If an error occurs, follow the proper protocol for corrections. Most electronic health record (EHR) systems allow for amendments with time stamps, ensuring transparency. Nurse practitioners should also refrain from documenting care that has not been provided.
6. Ensure Legibility and Readability
For paper charts, ensure that handwriting is clear and legible. With electronic documentation, use proper grammar, spelling, and punctuation to maintain professionalism and clarity.
7. Use Electronic Health Records (EHR) Effectively
Most healthcare settings rely on EHRs for charting and documentation. Nurse practitioners should familiarize themselves with their specific system’s features, including templates, shortcuts, and voice dictation tools. These functionalities can improve efficiency and accuracy in documentation.
8. Avoid Copy-Pasting Without Review
EHRs allow for copy-pasting previous notes, which can be helpful, but it’s essential to review and update each entry. Outdated or incorrect information can compromise patient safety and reflect poorly on clinical judgment.
9. Protect Patient Privacy and Comply with HIPAA
All charting and documentation must comply with the Health Insurance Portability and Accountability Act (HIPAA). Avoid including unnecessary personal details and never discuss patient records in unsecured or public settings. Additionally, always log out of EHR systems when not in use.
10. Document Patient Education and Informed Consent
A nurse practitioner must record patient education and discussions about informed consent. If a patient refuses treatment or deviates from recommendations, document the conversation, including the risks explained and the patient’s response.
11. Include a Complete Medication List
Accurate medication documentation is essential for preventing errors and interactions. Ensure that all prescribed, over-the-counter, and herbal medications are listed, along with dosages and frequencies.
12. Address Social Determinants of Health
Social and environmental factors can significantly impact patient health. When relevant, document issues like housing instability, food insecurity, or lack of transportation, as these factors can influence treatment plans and health outcomes.
13. Ensure Proper Coding and Billing Documentation
Charting and documentation directly impact coding and billing. Ensure that documentation supports the level of service provided to avoid claim denials or audits. Using the correct ICD-10 and CPT codes is crucial for appropriate reimbursement.
14. Document Changes in Patient Condition
If a patient’s condition changes significantly, update the documentation accordingly. A nurse practitioner should never assume that others will infer changes from previous notes.
15. Seek Continuous Improvement
Even experienced nurse practitioners can refine their charting and documentation skills. Attending workshops, reviewing institutional guidelines, and seeking mentorship can enhance efficiency and accuracy in documentation.
Common Charting and Documentation Pitfalls to Avoid
Over-Reliance on Templates
While templates streamline documentation, overusing generic phrases can lead to inaccuracies. Always personalize entries to reflect the specific encounter.
Vague or Incomplete Entries
Leaving out crucial details can lead to gaps in patient care. Ensure that documentation is thorough and that all pertinent findings and decisions are recorded.
Failure to Document Verbal Orders
When receiving verbal orders from other providers, document them accurately and ensure they are signed off according to institutional protocols.
Not Recording Missed or Declined Treatments
If a patient refuses a treatment or follow-up, document their reasoning and the counseling provided. This protects against potential liability claims.
Conclusion
Mastering charting and documentation is essential for every nurse practitioner. Not only does it enhance patient care and safety, but it also protects healthcare providers from legal and regulatory risks. By following best practices, such as using the SOAP format, documenting in real-time, and leveraging EHR tools effectively, nurse practitioners can ensure their records are accurate, comprehensive, and compliant.
Ultimately, strong charting and documentation habits lead to better communication, improved patient outcomes, and a more seamless workflow in clinical practice. Investing time and effort into refining these skills will pay off in the long run, benefiting both patients and practitioners alike.